In war-ravaged Ukraine, the rural elderly are especially vulnerable to illness. Many lack the technology, funds and confidence to connect with reliable medical providers. Others are homebound and can’t travel for care.
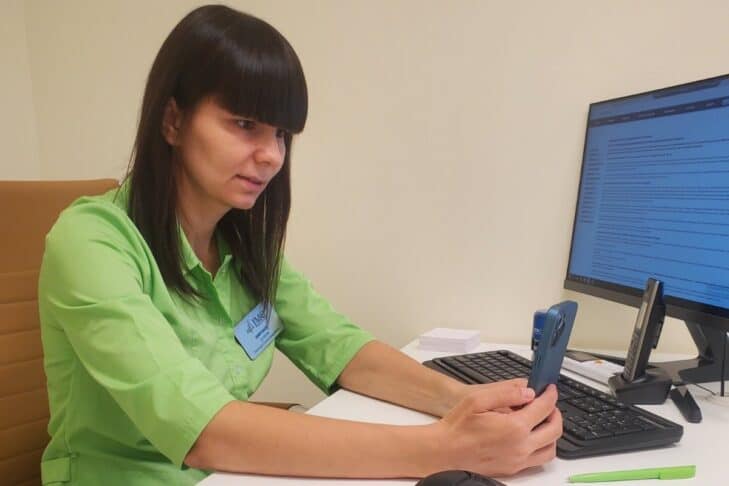
Action for Post-Soviet Jewry (APSJ) bridges the gap between isolated villagers and quality medical access with a growing telehealth program. Since its inception last year, with support from a CJP grant, it has provided dozens of elderly Ukrainians with care from clinicians from the Jewish Medical Center of Dnipro, a longtime CJP partner.
“We mostly serve aging Jews in smaller communities, who are harder to reach and lack robust services found in inner cities,” says APSJ executive director Debbie Kardon. “Health care in rural areas, especially for the elderly, is very difficult to get.”
APSJ has worked with vulnerable, elderly Ukrainian Jews for decades by offering humanitarian aid, services and supplies, now in 15 Ukrainian communities. The war created even more urgency, especially for Ukrainians 70 and older. This is a population that is often overlooked due to demographics, even more so now that the war has undermined crucial medical infrastructure. Many lack insurance; unlike in the United States, senior citizens don’t automatically qualify for health coverage.
Knowing that the Jewish Medical Center of Dnipro offered local telehealth services during COVID, APSJ approached them to expand their reach. A pilot program began, targeting seniors in Kryvyi Rih, Novomoskovsk, Pavlograd and Kamenskoye.
At first, Kardon wasn’t sure what to expect. Many elderly patients distrusted the medical establishment, she says. Others rarely used technology. But the program took off seamlessly.
“The [patients] had never done anything like this before. They come from the old Soviet Union, where medical treatment was very unsafe at times, and they had a lot of suspicions about it. To our surprise, within the first few weeks of us rolling this out in four communities, over 70 elders applied. The response was just unbelievable. It brings me to tears,” Kardon says.

Many elderly patients have been involved with APSJ in other capacities for many years. Volunteer coordinators already work in each affiliated community, attuned to residents who might be especially at risk, particularly those who live alone or who don’t receive support from other charitable organizations.
These coordinators then work with each prospective patient to complete paperwork, stay in touch with appointment reminders and ensure that they have a working phone for their visit. In some cases, it’s a video appointment; other times, it’s a phone conversation. The internet is often spotty in these rural villages, and volunteers play an essential part in confirming that physician and patient connect.
In many cases, care is long overdue: The majority of patients have never received comprehensive medical care and struggle with several ailments, such as heart disease or untreated diabetes. Often, physicians see a patient for one problem and discover several other illnesses in the process. Many complaints are war-related.
“In one instance, a woman’s building had been attacked by missiles. Her apartment had been shaken, and her window had been blown out. She had hit her head, and she had been bleeding. She was so anxious, her heart rate was so high, and she was able to have a consult with a neurologist,” Kardon says.
Just a couple of weeks ago, CJP provided additional funds to help reach more patients. In the future, Kardon hopes that more funding will supply patients with updated phones, equipped with video. She also hopes to scale the program further by expanding to more communities and subsidizing medication costs and equipment, such as glucose or blood pressure monitors.
“This project is really saving lives on so many levels. Now, elders feel incredibly cared for and, for the first time, they trust their providers,” she says.